
Prenatal diagnostics – DEGUM II (certification from the German Society of Ultrasound in Medicine)
Dear patient,
The news of becoming an expectant parent can be both joyful and at the same time raise worries about the health of your child. With the aid of prenatal diagnostics, we can support and advise you with modern ultrasound methods, blood tests and risk assessments. In our special consulting hours, we take plenty of time to advise you individually about the purpose of diagnostics and any consequences that may arise.
We would like to provide an overview of the current routine examinations in order to help you decide whether and to what extent you wish to take advantage of prenatal diagnostics.
The aim of the following is to give you some information prior to your individual consultation.
Together we will find out what is best for you and your child.
Dr Grit Neisser/Alexandra Selten
Specialist Doctors for Gynaecology and Obstetrics
Specialisation in prenatal diagnostics – DEGUM II
FMF London
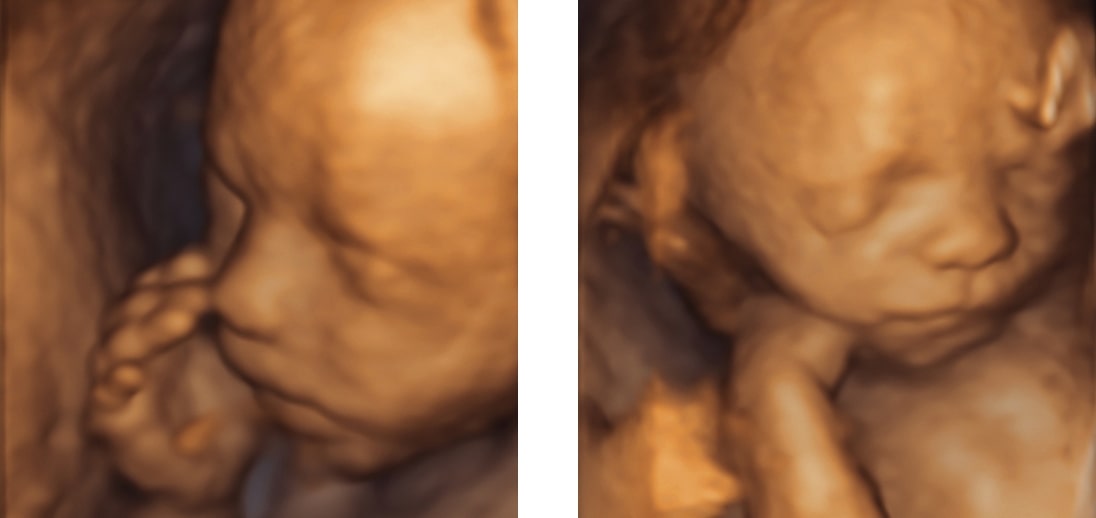

First trimester screening, 12th–14th week of pregnancy
Early anatomy ultrasound including nuchal fold measurement
(NT screening)
Measuring the nuchal fold at the back of the baby’s neck via ultrasound allows a probability calculation to estimate the individual risk for genetic diseases in the 12th to 14th week of pregnancy. The thicker the nuchal translucency (NT), the greater the risk that the child will suffer from potential diseases.
Based on this statistical probability calculation for trisomy 21, 13 and 18, you can decide for or against further invasive or non-invasive diagnostics (blood test, chorionic villus sampling or amniocentesis).
This ultrasound examination can also rule out severe birth defects at this early stage of pregnancy.
Biochemical risk assessment of chromosome disorders
Hormone testing of the mother’s blood can reveal characteristic changes in the concentration of parameters (e.g. PAPP-A, free ß-hCG) that are included in the risk calculation for genetic and morphological diseases in the first trimester screening. This increases the detection rate for genetic diseases in the child.
NIPT – non-invasive prenatal testing from the mother’s blood; trisomy 21, 18, 13
With this test, it is possible to detect the child’s DNA in the mother’s blood. The test is extremely accurate – more than 99% for trisomy 21, which is much higher than the probability calculation from the first trimester screening. This blood test does not replace the early anatomy screening, as only a targeted ultrasound examination can detect or rule out many foetal conditions, developmental disorders or deformities. These are not necessarily related to the trisomies discussed above.
Anatomy scan including foetal echocardiogram, 22nd–23rd week of pregnancy
We use our high-resolution ultrasound system to examine your child’s growth, organ development, the function and anatomy of the heart (foetal echocardiogram) and blood supply (Doppler sonography). This allows us to assess the physical development of the unborn child. The foetal echocardiogram can rule out a large number of heart defects. In the majority of cases, this examination of the pregnant woman confirms that the child is developing normally.
Doppler sonography
Doppler sonography allows us to measure the blood flow in the foetal blood vessels, the umbilical cord and the blood vessels in the mother’s uterus. Using this, we can recognise risk factors for growth restrictions of the child and pregnancy-related illnesses.
